
imPACT: July 2020
Message from the Chair 
I’m not even going to say the word, suffice to say the ‘imPACT’ has been almost unimaginable. The first few cases were only just emerging when I last wrote to you and now the world has changed forever. The impact on clinical trial activity has been very significant – more on that later – but one of the legacies of the pandemic, aside from the disappearance of the handshake and a doubling in household toilet paper inventories, will be much greater awareness of the role and importance of clinical trials and the networks which drive them in generating the new knowledge which improves and saves lives. All of a sudden ‘randomisation’ and ‘statistical power’ are household words. Even prominent politicians are designing clinical trials these days.
The other side of the pandemic which I have found remarkable is the capacity for clinical trial activity to dramatically accelerate when there is political and social pressure. New collaborations have formed overnight, regulatory roadblocks have disappeared, and red tape has been brushed aside. I know many of my patients, and I’m sure many of you, are frustrated by the slow pace of drug discovery in IPF and other progressive fibrosing ILDs. Let’s hope some of these changes stick around when the virus has been beaten back.
Professor Dan Chambers,
PACT Chair
Message from the CRE-PF
 Our objective at the Centre of Research Excellence in Pulmonary Fibrosis (CRE-PF) is to improve and extend the lives of patients living with pulmonary fibrosis Australia-wide, through a comprehensive and integrated program of basic and clinical research and education. During these uncertain times amidst the COVID-19 pandemic, we have we have necessarily suspended some research activities whilst our respiratory health professionals are called to the frontline of the COVID-19 clinical response in Australia. However, we are pleased to report that the NHMRC has now extended the CRE-PF grant for 12 months. Fortunately, as the clinical situation improves, the CRE-PF has now been able to transition from our initial response into a recovery phase of increasing research activity.
Our objective at the Centre of Research Excellence in Pulmonary Fibrosis (CRE-PF) is to improve and extend the lives of patients living with pulmonary fibrosis Australia-wide, through a comprehensive and integrated program of basic and clinical research and education. During these uncertain times amidst the COVID-19 pandemic, we have we have necessarily suspended some research activities whilst our respiratory health professionals are called to the frontline of the COVID-19 clinical response in Australia. However, we are pleased to report that the NHMRC has now extended the CRE-PF grant for 12 months. Fortunately, as the clinical situation improves, the CRE-PF has now been able to transition from our initial response into a recovery phase of increasing research activity.
Fortunately, many of the CRE-PF research activities including our epidemiology group (Menzies Institute) and discovery science (University of Western Australia) are unaffected by the clinical situation and will continue as planned. Many suspended clinical phenotyping research projects have resumed, including work on connective tissue disease related pulmonary fibrosis and idiopathic pulmonary fibrosis. We’ve taken proactive steps to protect our ability to deliver outputs and achieve research aims, and to position ourselves for rapid resumption of suspended activities once the situation improves.
We remain active across the domains of translation and education, clinical trials, researcher development, epidemiology and health economics, clinical phenotyping and discovery science research. We are already utilising our network to contribute to COVID-19 education and research, flexibly responding as the situation develops. In the last few months, we have delivered COVID-19 webinars for people living with PF on topics including staying safe during the pandemic, looking after your mental health and staying fit and strong at home and a COVID-19 resource factsheet for people living with pulmonary fibrosis. In addition to the existing CRE-PF research projects, we have recently been able to commence work on a number of strategic projects to help shape the future of PF research in Australia. One of these is a national research project investigating the impact of COVID-19 on people living with pulmonary fibrosis.
We will continue to actively support our network during these rapidly changing times and remain committed to achieving the aims of our research program throughout this challenging time and beyond.
Yours sincerely,
A/Prof Tamera Corte
CIA for CRE-PF
Trials Update
It has required some quick thinking, a dose of ingenuity and amazing understanding and patience from those participating in clinical trials, but most activity has managed to continue in Australia and New Zealand, although many trials were closed to new recruitment, and several trials have been put ‘on-hold’. Things are now opening up around the world, but particularly in Australia and New Zealand and so global trial leads are now looking to us to re-double our efforts to recruit. The only PACT trial which remains closed to recruitment is TRAIL – pirfenidone in rheumatoid arthritis-associated ILD. All our other trials are open, but not all PACT centres are recruiting yet so check with us or your local team. Trials which are actively recruiting are listed here. Excitingly, several new trials will be listed soon, so keep checking in.
Grants
The second annual PACT Grant-in-Aid for Investigator Led Pulmonary Fibrosis Clinical Research has been delayed by the pandemic. Provided things remain clinically improved in Australasia (touch wood), we will open applications later in the year.
We are thrilled to be able to share that recently there has been some exciting and hard-fought grant funding success for pulmonary fibrosis research. Congratulations to:
- Dan Chambers and the national collaborative team for “The TELO-SCOPE Study: Attenuating Telomere Attrition with Danazol. Is there Scope to Dramatically Improve Health Outcomes for Adults and Children with Pulmonary Fibrosis?” funded through the MRFF RCRDUN initiative
- Anne Holland for her NHMRC Investigator Grant “Optimising patient & health system outcomes in chronic respiratory disease”
- Natasha Smallwood for her NHMRC Investigator Grant “Targeted approaches to improve health outcomes in severe respiratory disease”
- Sionne Lucas and the national GRIPF team for “Genetic Research in Idiopathic Pulmonary Fibrosis (GRIPF) Study: A case-control cohort enriched for genetic disease” to extend the reach of the original study and include a case-control cohort, funded through Perpetual’s IMPACT Philanthropy Program
- The Graham Painton Fellowship awarded to Ashleigh Philp working on “Understanding pathogenesis to develop new treatments for IPF” who joins Phil Hansbro and his team spanning UNSW and UTS.
Upcoming Events of Interest
As with so many things in 2020, pulmonary fibrosis conference and event plans have been upended. The ERS International Congress is going completely virtual this year – the innovative and interactive event will take place 7-9 September, registrations are now open.
ICLAF 2020 was scheduled for 3-7 October in Reykjavik, Iceland. While we’re still waiting for the official word, it is anticipated that this will have to be delayed to 2021 due to safety issues and travel restrictions. Keep an eye on their website for updates.
Meanwhile, the CRE-PF team have kicked off Australasian Pulmonary Fibrosis Virtual Research Meetings to promote collaboration and discussion amongst Australasian researchers interested in pulmonary fibrosis. Our second monthly virtual research meeting will take place Friday 17th July at 12-1pm AEST, featuring the team at the Menzies Institute for Medical Research, University of Tasmania. Join us on Zoom https://uni-sydney.zoom.us/j/97081853167.

Membership
The PACT network continues to build our membership and welcomes new members across all aspects of pulmonary fibrosis clinical research, care and support. We invite you to encourage your colleagues to join our growing community by completing the form below.
Become a memberFive Minutes with a Pulmonary Fibrosis Researcher
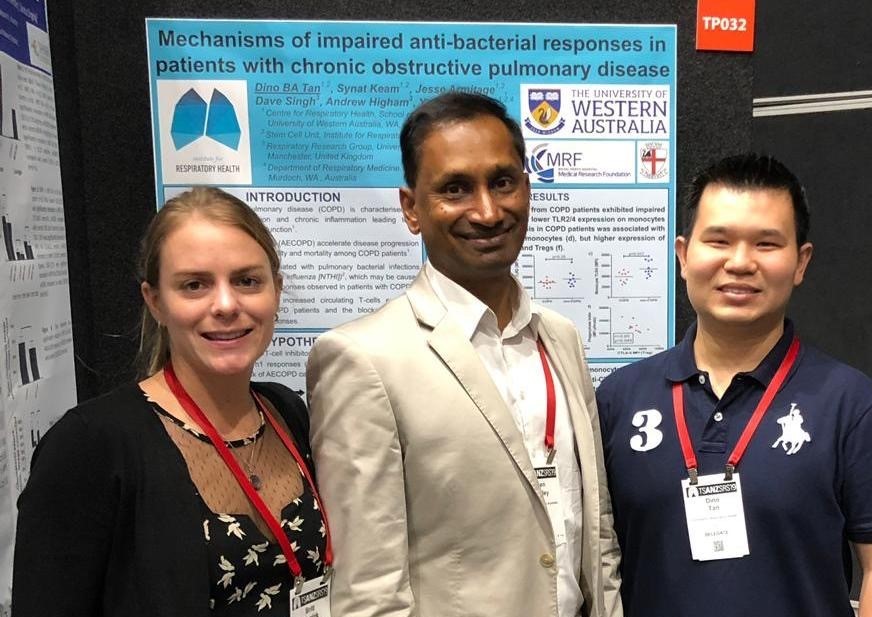
A/Prof Yuben Moodley, Fiona Stanley Hospital and University of Western Australia
A/Prof Moodley sat down with the PACT team to talk about his teams clinically focussed research, including how it started, what the team hopes it will achieve and the challenges they’ve faced.
Tell us a bit about yourself and why you chose Pulmonary Fibrosis (PF) as your research area:
I am a Respiratory Physician at Fiona Stanley Hospital and Clinical Academic at the University of Western Australia. In addition, I am Senior Editor of the journal Respirology and Deputy Director of the Institute of Respiratory Health. Lung diseases are a very important cause of global morbidity and mortality. As a physician I am acutely aware that significant lung damage leads to shortness of breath all day with no reprieve. This is a very difficult form of suffering and requires urgent solutions to preserve lung function. Pulmonary fibrosis is the end-stage of several pathways of lung damage. Understanding the mechanisms and “curing” pulmonary fibrosis is one of the holy grails of medicine.
Describe your clinical research project in a couple of sentences:
We are carrying out several projects in translational and discovery science in pulmonary fibrosis. One of the NHMRC funded projects identifies the markers in blood that would predict which patients would decline in their lung function versus those patients that would remain stable. We are also determining which markers in blood would predict patients would respond to anti-fibrotic treatment. This is important since we can avoid using expensive treatments with significant side-effects, if patients are not going to respond to certain treatments. Furthermore, these blood markers will give us insights into the molecular processes in the lung that would determine what pathways are responsible for the decline in lung function at the tissue level.
Tell us how this project came about:
The Australian Idiopathic Pulmonary Fibrosis (IPF) Registry was the foundation on which we built our national infrastructure. This resource gave us the opportunity to seek funding for pulmonary fibrosis research. As such we were able to collect blood from our patients on the registry and determine the demographics and trajectory of their lung function. We then correlated their blood markers with these demographics and treatment. Our CRE also allowed us to set up a tissue bank that provides us with IPF lung tissue to determine the role of these markers in tissue.
What do you hope this project will achieve?
We will find blood markers that will be used in clinics around the world that would determine patients who have more serious disease versus those who are stable.
With the rapid increase in medications for pulmonary fibrosis, we hope to develop a clinical test that would allow us to determine which patients would respond to specific therapeutic agents thus allowing doctors to “personalise” treatment for pulmonary fibrosis patients.
We hope to identify unique mechanisms of progression at the level of lung tissue damage in pulmonary fibrosis thus leading to new targets for treatment.
What has been the biggest challenge of the project so far?
Funding is the biggest challenge and the collection of blood samples to a lesser extent. The latter has been overcome by a truly national effort to obtain blood and this is succeeding. If we had more money, we could do so much more, so much more quickly.
The people working on this project are:
Dr Britt Clynick and Dr Dino Tan are post-doctoral scientists working on the scientific aspects of this project. Ms Chantalia Tejda is working in the blood biobank. We have a national collaboration of the members of the Australian IPF Registry and physicians from all the major sites.
What do you see as the biggest evidence gaps in PF care? What are the clinical research priorities?
Why and how people get pulmonary fibrosis. The mechanisms causing pulmonary fibrosis and its progression. We should be looking at the identification and treatment of early lesions that may prevent end-stage lung disease.